03. diseases of thyroid gland
- 1. DISEASES OF THE THYROID GLAND Fahad zakwan MD5 2014
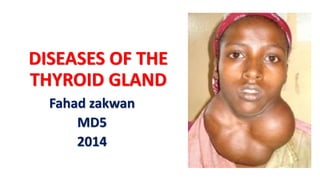
- 2. INTRODUCTION • Diseases of the thyroid gland invariably leads to enlargement of the gland. • The term GOITER is applied to any enlargement of the thyroid gland regardless of the cause. • These diseases can be classified into different categories using the following schema.
- 3. Causes of thyroid disease inflammatory Acute Subacute chronic toxic Primary secondary autoimmune Hashimoto Reidel thyroiditis simple Physiological Colloidal nodular neoplastic Benign malignant
- 4. 1. Simple goiter • There is chronic deficiency of Thyroxine (T4) and or triiodotrynine (T3) in the body which in turn causes compensatory elevation of TSH because of the lack of necessary negative feedback. • Prolonged stimulation of TSH in attempt to bring normal thyroid hormones level leads to simple goiter. • Such phenomenon may occur in the following settings; • Iodine deficiency, • environmental or physiological e.g. pregnancy, • Enzymatic deficiency for example in Pendred’s syndrome which is caused by peroxidase deficiency,
- 5. Classification of simple goiter •Simple goiters are of three types; •simple diffuse goiter •simple colloid goiter •simple nodular goiter
- 6. Pathophysiology • Chronic absence of T4/T3 causes elevated level of TSH, which then leads to diffuse homogenous hypertrophy and hyperplasia of follicular cells and colloid (secretory follicles) in efforts to produces more thyroid hormones. • This is usually a reversible change. • The enlarged thyroid hyper involuted with colloid is called colloid goiter. • Differential response to TSH leads to formation of nodules within the gland.
- 7. Pathophysiology • Several nodules may coalesce and lead to formation of multinodular goiter. • The nodules may undergo secondary changes; central necrosis, cystic degeneration, hemorrhage, calcification and malignant changes (3%). • In about 30% of patients, a very huge goiter may secret excess hormones and lead to secondary hyperthyroidism, this is not classified as simple goiter.
- 8. Clinical presentation • Gradual onset of painless anterior neck swelling, usually long standing in endemically iodine deficient areas. • Recent onset of pain or increase in size may indicate secondary changes. • The enlarged gland may also affect neighboring structures and lead to wide range of symptoms and signs. • Obstruction of airways may lead to difficulty in breathing, wheezing, and cough on lying supine.
- 9. Clinical presentation • Laryngeal nerve compression or involvement by cancer can lead to horsiness of voices. • Esophageal obstruction or involvement by cancer can lead to dysphagia. • Neck veins obstruction can lead to facial congestion or plethora, congested neck and face veins, and superior vena cava syndrome in huge retrosternal goiters. • Superior vena cava syndrome tends to be worse when a patient raises arms above the head (Pemberton’s sign). • A huge goiter is also considered uncosmetic by most people. • Lastly but not least, patient may also present with symptoms of hypo or hyper thyroidism (to be discussed later).
- 10. Investigation in simple goiter Thyroid function test • Thyroid function test measures serum levels of: • thyroxine (T4), • tri iodothyronine (T3), • thyroid stimulating hormones (TSH) • thyrotropin releasing hormone (TRH). • This helps to know if the thyroid gland is normally, hyper or hypo functioning.
- 11. Thyroid scan with radioactive iodine (I123 or I131) • In this investigation a traceable radioactive Iodine or Technetium is injected into the blood stream, the thyroid gland concentrates radioactive iodine. • The concentrated radioactive iodine can be detected by gamma camera or scintillation counter. • I123 has a shorter half life as compared to I131 and therefore preferred because it has less exposure of the patient to radiation. • Thyroid scan may show hot nodules (which takes more radioactive iodine than the rest of gland) in secondary hyperthyroidism, however most simple goiters have normal uptake or Cold nodules (which does not take radioactive iodine). • Cold nodules are likely to be malignant.
- 13. Antithyroid receptors antibodies •This type of investigation is done in patients suspected to have stimulatory auto antibodies as is the case in Grave’s disease (primary hyperthyroidism).
- 14. Radiological investigations • Normal AP and lateral chest X-rays may demonstrate retrosternal extension of the goiter (retrosternal shadow), but also rules out other chest problems.
- 15. • Thoracic inlet X-rays may demonstrate compression or deviation of the trachea, this important to anesthetist if surgery is contemplated (difficult intubation).
- 16. •Computed tomography may be indicated if more details are needed before surgery or there is suspicion of malignancy transformation.
- 17. Fine needle aspiration cytology • Is one of the very important investigations to rule out malignancy of thyroid. Results can be; • malignant, • suspicious malignant, • benign, • inconclusive or inadequate aspirate. • If follicular pattern is seen, lobectomy is done to exclude follicular carcinoma, because the can only be differentiated by demonstrating capsular invasion.
- 18. Treatment and prevention of simple goiter Dietary and Medical • Iodine supplementation in iodine deficient areas, food iodine fortification is one of the best preventive measures of goiters. Thyroxin supplementation • In patients with diffuse hyperplastic goiter for several months (0.1 to 0.2mg per day).
- 19. Surgery indicated In the following features; •in patients with obstructive symptoms, •when malignancy is suspected clinically or after FNAC, •hyper functioning nodules •for cosmetic reasons
- 20. 2. Toxic goiter, thyrotoxicosis or hyperthyroidism • Hyperthyroidism is a condition in which an overactive thyroid gland is producing an excessive amount of thyroid hormones that circulate in the blood. • Thyrotoxicosis is a toxic condition that is caused by an excess of thyroid hormones from any cause. • Thyrotoxicosis can be caused by an excessive intake of thyroid hormone or by overproduction of thyroid hormones by the thyroid gland. • Hyperthyroidism can be primary or secondary depending on the etiology.
- 21. Causes of hyperthyroidism Some common causes of hyperthyroidism include: • Graves' Disease • Functioning adenoma ("hot nodule") and toxic multinodular goiter (TMNG) • Excessive intake of thyroid hormones • Abnormal secretion of TSH • Thyroiditis (inflammation of the thyroid gland) • Excessive iodine intake
- 22. Primary hyperthyroidism Grave’s disease • Graves’s disease is an autoimmune disease of the thyroid gland, in which there is a circulating autoantibody which resembles TSH. • The autoantibody binds to and stimulates G-protein coupled thyrotropin receptors on thyroid gland leading to thyroid hormone release and hyperplasia. • These antibodies include • thyroid stimulating immunoglobulin (TSI antibodies), • thyroid peroxidase antibodies (TPO), and • TSH receptor antibodies
- 23. •These antibodies also react with retrobulbar auto antigens to cause periorbital edema and protrusion of eye ball (exophthalmos). •Graves' disease is hereditary and is up to five times more common among women than men • Female: male ratio is 9:1 • Grave’s disease tends to affect young than older women • It causes about two third of all cases of hyperthyroidism
- 24. •The triggers for Grave's disease include: •stress, •smoking, •radiation to the neck, •medications, •Infectious organisms such as viruses.
- 25. Secondary hyperthyroidism • In patients with secondary hyperthyroidism, there is a pre existing thyroid pathology for example goiter or inflammatory condition which leads to excess production of thyroid hormones or there is an extra thyroid source of hormone production. • Secondary hyperthyroidism has high predilection to involve cardiovascular system as discussed under clinical features below.
- 26. Multinodular goiter •In this form of secondary hyperthyroidism, there is hypersecreting toxic nodule in the background of multinodular goiter (Plummer’s disease); •this tends to occur in iodine deficient areas (endemic goiters).
- 27. Toxic adenoma •This form of secondary hyperthyroidism is characterized by presence of benign glandular nodule in the thyroid gland, usually follicular which secrets excess hormones.
- 28. Ectopic thyroid hormone • In this form of secondary hyperthyroidism, there is a hormone producing tumor elsewhere in the body. • For example metastatic follicular thyroid carcinoma, choriocarcinoma which produces β-hCG whose alpha chain resembles TSH and thyroid tissue containing teratoma. • The excess thyroid hormones lead to clinical features typical of hyperthyroidism.
- 29. Exogenous causes •In this form, excess hormone has been introduced into the body. •An example is what is called thyrotoxicosis factitious which is due to excess intake of thyroxine hormone and Jod-Basedow which is caused by excessive intake of iodine in endemic goiter.
- 30. TSH producing pituitary adenoma •This is another cause of excess thyroid hormone production; an adenoma in the pituitary gland (which normally controls the thyroid gland) produces TSH which in turn leads to excess T4 and T3.
- 31. Other causes • Other causes include • post viral thyroiditis with transient self limiting thyrotoxicosis (Subacute de Quervain’ thyroiditis); this form of hyperthyroidism is usually painful and may be associated with other systemic symptoms. • Radiation induced thyroiditis with release of preformed thyroid hormones is commonly seen in patients undergoing neck radiation
- 32. Thyroiditis • Inflammation of the thyroid gland may occur after a viral illness (Subacute thyroiditis). • This condition is associated with a fever and a sore throat that is often painful on swallowing. • The thyroid gland is also tender to touch. • There may be generalized neck aches and pains. • Inflammation of the gland with an accumulation of white blood cells known as lymphocytes (lymphocytic thyroiditis) may also occur.
- 33. Clinical features Central nervous system symptoms; • Central nervous system features are very common in patients with primary thyrotoxicosis. • Features commonly seen are: • tremors which can be observed on the tongue and fingers, • nervousness, • emotional liability (patients become irritated easily), they may also be lethargic or agitated and usually they have warm and moist hands.
- 34. Increased metabolic rate; •Feature falling under this category include; •heat intolerance, •weight loss, •excessive sweating, and •tiredness cause by muscle weakness as a result of proteolysis.
- 35. Cardiovascular; • This category of clinical features is very common in patients with secondary hyperthyroidism. • They include • awareness of heart beats (palpitation) due to tonic and chronic effect of excess thyroid hormones, • irregular heartbeats (arrhythmia), • sleeping tachycardia, • high output heart failure and • thyroid bruit due to excess blood flow to the gland.
- 36. Gastro intestinal tract (GIT); •Gastro intestinal features which can be seen in patients’ hyperthyroidism are: •loss of body weight despite having good or increased appetite, and •increase bowel motions (diarrhea).
- 37. Genital urinary tract (GUT) •In the genital urinary system, hyperthyroidism can lead to •irregular menstruation, •amenorrhea, •loss of libido and •erectile dysfunctions
- 38. Eye or ophthalmological features • Eye symptoms as is the case for central nervous system are very common in Grave’s disease. • Eye protrusion or exophthalmos can be true when it is caused by retrobulbar cellular infiltration and mucopolysaccharide depositions or false exophthalmos when it is caused by elevation of superior eye rid due to due to hyper activity of levator pulpebral superioris muscle or
- 40. •Exophthalmos can lead to •exposure conjunctivitis, •keratitis (corneal ulceration) and •perforation. •Ophthalmoplegia or eye paralysis can be caused by cellular infiltration. •Ophthalmoplegia can be bilateral or unilateral and can be associated with diplopia (double vision).
- 41. The summary of clinical features is presented in tabular form below; Clinical features Primary Hyperthyroidism (Grave’s) Secondary Hyperthyroidism (Plumer) Age Young age Elderly Onset Abrupt Gradual Course Remissions & exacerbations Steady course Nervous symptoms +++ + Metabolic manifestations +++ + Eye signs +++ FALSE CV manifestations + +++ Thyroid gland Diffuse Nodular
- 42. Thyroid storm (thyrotoxic crisis) • A rare presentation of thyrotoxicosis, there is extreme signs of thyrotoxicosis associated with severe metabolic disturbances. • It occurs in patient with hyperthyroidism who has not been well prepared (hyperthyroidism is not controlled) before surgery. • It may also occur in patients with major stress eg major trauma and infection. • Clinical features includes; • hyper-thermia, • tachycardia, • irritability, • profuse sweating and • diarrhea.
- 43. Treatment of thyrotoxicosis •There are three main forms of treatment for thyrotoxicosis; 1. Medical treatment 2. Symptomatic treatment 3. Antithyroid treatment
- 44. Medical treatment • In this form of treatment, patients are given medications which either target the thyroid hormones or symptoms. • Indications include; • primary thyrotoxicosis in small gland, • primary thyrotoxicosis in young age, • pre-operative preparation, • post-operative recurrence and • patient’s refusal of surgery.
- 45. Symptomatic treatment • This targets central nervous system and cardiovascular symptoms. • Beta adrenergic blockers are the mainstay of symptomatic therapy for thyrotoxicosis. • propranolol in range of 40mg twice or thrice a day has been used with greatest success due to additional benefit of inhibition of peripheral conversion of T4 to T3 • D-propranolol is a beta blocker and therefore reduces tachycardia, anxiety, insomnia, diarrhea and other symptoms.
- 46. • Fevers are treated with cooling measures and antipyretics. • However aspirin should be avoided to prevent decreased protein binding and subsequent increases in the free T3 and T4 levels. • Intravenous glucocorticoids are indicated if adrenal insufficiency is suspected. • Large doses of dexamethasone (2mg q6h) inhibit hormone production and decrease peripheral conversion from T4 to T3. • Aggressive hydration of up to 3 – 5 L/d of crystalloid compensates for potentially profound GI and insensible losses. • Charcoal hemoperfusion has been shown to be effective in treatment of iatrogenic or intentional ingestion of excessive doses of levothyroxine
- 47. Antithyroid treatment • These drugs either blocks iodine binding to tyrosine and decrease antibody titers (Carbimazole) or block iodine binding and prevent conversion of T4 to T3 (propylthiouracil). • Both drugs are fairly effective and fairly safe in pregnancy, except that carbimazole may cause fetal aplasia cutis and therefore may be avoided in pregnancy. • Carbimazole can cross placenta more than thyroxin and it also crosses breast milk and therefore avoided in pregnancy and lactating mothers, although can be used if dose is less than 20mg.
- 48. •Antithyroid drugs are grouped into: •Inhibitors of hormone synthesis •Propylthiouracil (PTU) •Methimazole (Tapazole) •Blockade of hormone release •Lopanoic acid •Saturated solution of potassium iodide •Lugol solution
- 49. Propylthiouracil (PTU) • The drug of choice • Effects may be seen soon after the drug is started, but therapy may need to be continued for 4 – 12 weeks. • Recommended as DOC for women who are pregnant or breastfeeding. • Dosage: • HYPERTHYROIDSM: • 300 – 450 mg/day 8 hrly initially (may require up to 600 – 900 mg/day) • Maintenance: 100 – 150 mg/day 8hrly
- 50. • THYROTOXIC CRISES: • Initial 200 – 300 mg PO q4 – 6hr initially on day 1 (may require 800 – 1200mg/day), • Then reduce gradually • Some practitioners propose an initial dose of 600 – 1000mg with gradual dose reduction after initial response. • Maintenance: 100 – 150mg/day PO divided q8 – 12hr • GRAVES DISEASE: • 50 – 150mg PO initially • Maintenance: 50mg PO q8 – 12hr for up to 12 – 18 months, then taper and discontinue if TSH is normal
- 51. Surgical treatment • All patients must be euthyroid before embarking in surgery, ECG, CXR, and Echocardiogram must be done to rule out arrhythmia and heart failure. • Thoracic inlet X-ray in huge goiters to rule tracheal deviation and compression as discussed above. • Lugol’s iodine reduces risk of hemorrhage.
- 52. Indications for surgical intervention Surgical intervention is indicated in the following conditions; 1. Graves disease in young, 2. large gland or in patients with exophthalmos, 3. multi-nodular or solitary nodule, 4. unresponsive, poor compliance to medical treatment and when there is contraindication to drug e.g. hypersensitivity.
- 53. Types of surgery • Subtotal thyroidectomy; leaves about 8-10 gram of thyroid tissue, either 4- 5gram on each side or 8-10 gram on one side. The later is preferred because it makes reoperation easier. • Near total thyroidectomy removes nearly all thyroid tissue leaving only about 4gm thyroid tissue; • Partial lobectomy removes only half of the thyroid lobe; • Lobectomy removes the entire lobe one side with isthmusectomy eg in solitary toxic nodule; • Partial thyroidectomy; bilateral partial lobectomy eg in multinodular toxic goiter involving both lobes.
- 56. Complication of thyroid surgery Hemorrhage • Hemorrhage is one of the most common complications following thyroid gland surgery. There are three types of hemorrhage in patients who has undergone thyroid surgery; • Primary is a type of bleeding which occur during surgery due to arterial or venous cut, • Reactionary bleeding occurs when a patient’s blood pressure comes to normal after waning of hypotensive anesthetic drugs or due to pain and • Secondary bleeding which occurs 7 days to 2 weeks after surgery, usually due to infection of wound.
- 57. •Any form of bleeding may lead to hematoma in the neck which in turn can lead to upper airway obstruction. •Sometimes the blood is no visible as it percolates into the mediastinum, this is potentially dangerous because it is difficult to detect.
- 58. Respiratory obstruction • Apart from hematoma formation, the following can also cause airway obstruction post thyroidectomy period; • traumatic laryngeal oedema, • bilateral recurrent laryngeal nerve injury leading to vocal cords paralysis, especially in patients with huge thyroid complicated by difficult surgery, • tracheomalacia occurs in patients with huge goiters or those with retrosternal extension.
- 59. Recurrent laryngeal nerve injury •Recurrent laryngeal nerve injury can be •unilateral leading to hoarseness of voice & dyspnea on exertion, •bilateral incomplete in which the patient can present with stridor (due to irritation of adductor fibers) •bilateral complete with voice loss (aphonia).
- 60. Superior laryngeal nerve damage •Superior laryngeal nerve injury may also occur in difficult surgery, •loss of function of this nerve leads to loss of high pitched voice (cricopharyngius paralysis).
- 61. Thyroid insufficiency •Thyroid insufficiency following thyroidectomy may occur 2 to 5 years later, it may occurs as high as 20 to 45% in patients who have undergone total thyroidectomy.
- 62. Parathyroid insufficiency • Hypoparathyroidism occurs when both parathyroid glands are accidentally traumatized, devascularized or damaged. • If seen after removal, the glands must be reimplanted on deltoid muscles or sternocleidomastoid muscles. • The incidence of hypoparthyroidisim occurs in less than 0.5% of all patients underwent thyroidectomy. • Remember that parathyroid hormone is responsible for calcium homeostasis (increases GIT calcium reabsorbtion, resorbs bone, reduces renal calcium excretion and enhances phosphorus renal excretion). In absence causes hypocalcaemia.
- 63. Keloid scar and hypertrophic scars •Keloid and hypertrophic scars are late complication of thyroidectomy, occurring several years after surgery. •The two can be differentiated because the former forms mass which crosses an incision line and the later does usually cross the incision line.
- 65. Management of some important post operative complications Hematoma and bleeding • This is one of the most common complications in thyroid surgery. When suspected, reopen the wound immediately and ligate any bleeding vessel (wound exploration and bleeder ligation). • Such treatment should start at bed side if bleeding is severe or when hematoma is obstructive. • Give IV fluids using large bore canular and transfuse if necessary.
- 66. Respiratory obstruction and recurrent laryngeal nerve damage •Intubate the patient immediately if obstruction is severe, or •perform cricothyroidotomy if intubation is not convenient. •Ventilate or give high flow oxygen 8 L/second and make sure an intravenous line is established with crystalloids.
- 67. Hypoparathyroidism •Symptoms and signs of hypocalcaemia include circumoral paresthesias, mental status changes, tetany, carpopedal spasm, laryngospasm, seizures, QT prolongation on ECG, and cardiac arrest. •In such condition, a patient is given IV 10mls of 10% Calcium Gluconate over 10 minutes, or calcium carbonate 2.5g to 5g orally.
- 68. Thyroid storm •Supportive measures which includes IV fluids ice packs and antipyretics, oxygen mask 8litres per second, and sedatatives. •Specific treatment include giving propranolol 1mg IV as drip repeated if needed, oral Carbimazole or propylthiouracil and Digoxin if heart failure is diagnosed.
- 69. 3. HYPOTHYROIDSM • Hypothyroidism is a condition characterized by abnormally low thyroid hormone production. • There are many disorders that result in hypothyroidism. • These disorders may directly or indirectly involve the thyroid gland. • Because thyroid hormone affects growth, development, and many cellular processes, inadequate thyroid hormone has widespread consequences for the body.
- 70. Causes: • Hashimoto's thyroiditis • Lymphocytic thyroiditis (which may occur after hyperthyroidism) • Thyroid destruction (from radioactive iodine or surgery) • Pituitary or hypothalamic disease • Medications • Severe iodine deficiency
- 71. Hashimoto's thyroiditis • In this condition, the thyroid gland is usually enlarged (goiter) and has a decreased ability to make thyroid hormones. • Hashimoto's is an autoimmune disease in which the body's immune system inappropriately attacks the thyroid tissue. In part, this condition is believed to have a genetic basis. • This means that the tendency toward developing Hashimoto's thyroiditis can run in families • Hashimoto's is 5 to 10 times more common in women than in men
- 72. • Blood samples drawn from patients with this disease reveal an increased number of antibodies to the enzyme, thyroid peroxidase (anti-TPO antibodies). • Since the basis for autoimmune diseases may have a common origin, it is not unusual to find that a patient with Hashimoto's thyroiditis has one or more other autoimmune diseases such as diabetes or pernicious anemia (B12 deficiency). • Hashimoto's can be identified by detecting anti-TPO antibodies in the blood and/or by performing a thyroid scan.
- 73. Lymphocytic thyroiditis following hyperthyroidism • Thyroiditis refers to inflammation of the thyroid gland. When the inflammation is caused by a particular type of white blood cell known as a lymphocyte, the condition is referred to as lymphocytic thyroiditis. • This condition is particularly common after pregnancy and can actually affect up to 8% of women after they deliver. • In these cases, there is usually a hyperthyroid phase (in which excessive amounts of thyroid hormone leak out of the inflamed gland), which is followed by a hypothyroid phase that can last for up to six months. • The majority of affected women eventually return to a state of normal thyroid function, although there is a possibility of remaining hypothyroid.
- 74. Thyroid destruction secondary to radioactive iodine or surgery • Patients who have been treated for a hyperthyroid condition (such as Graves' disease) and received radioactive iodine may be left with little or no functioning thyroid tissue after treatment. • The likelihood of this depends on a number of factors including the dose of iodine given, along with the size and the activity of the thyroid gland. • If there is no significant activity of the thyroid gland six months after the radioactive iodine treatment, it is usually assumed that the thyroid will no longer function adequately. The result is hypothyroidism. • Similarly, removal of the thyroid gland during surgery will be followed by hypothyroidism.
- 75. Pituitary or Hypothalamic disease • If for some reason the pituitary gland or the hypothalamus are unable to signal the thyroid and instruct it to produce thyroid hormones, a decreased level of circulating T4 and T3 may result, even if the thyroid gland itself is normal. • If this defect is caused by pituitary disease, the condition is called "secondary hypothyroidism." • If the defect is due to hypothalamic disease, it is called "tertiary hypothyroidism."
- 76. Pituitary injury • A pituitary injury may result after brain surgery or if there has been a decrease of blood supply to the area. In these cases of pituitary injury, the TSH that is produced by the pituitary gland is deficient and blood levels of TSH are low. • Hypothyroidism results because the thyroid gland is no longer stimulated by the pituitary TSH. This form of hypothyroidism can, therefore, be distinguished from hypothyroidism that is caused by thyroid gland disease, in which the TSH level becomes elevated as the pituitary gland attempts to encourage thyroid hormone production by stimulating the thyroid gland with more TSH.
- 77. Severe iodine deficiency: •In areas of the world where there is an iodine deficiency in the diet, severe hypothyroidism can be seen in 5% to 15% of the population.
- 78. Symptoms of hypothyroidsm • The symptoms of hypothyroidism are often subtle. They are not specific (which means they can mimic the symptoms of many other conditions) and are often attributed to aging. • Patients with mild hypothyroidism may have no signs or symptoms. • The symptoms generally become more obvious as the condition worsens and the majority of these complaints are related to a metabolic slowing of the body.
- 79. Common symptoms are listed below: • Fatigue • Depression • Modest weight gain • Cold intolerance • Excessive sleepiness • Dry, coarse hair • Constipation • Dry skin • Muscle cramps • Increased cholesterol levels • Decreased concentration • Vague aches and pains • Swelling of the legs
- 80. • As the disease becomes more severe, there may be puffiness around the eyes, a slowing of the heart rate, a drop in body temperature, and heart failure. • In its most profound form, severe hypothyroidism may lead to a life-threatening coma (myxedema coma). • In a severely hypothyroid individual, a myxedema coma tends to be triggered by severe illness, surgery, stress, or traumatic injury. • This condition requires hospitalization and immediate treatment with thyroid hormones given by injection.
- 81. diagnosis • A diagnosis of hypothyroidism can be suspected in patients with fatigue, cold intolerance, constipation, and dry, flaky skin. • A blood test is needed to confirm the diagnosis. • When hypothyroidism is present, the blood levels of thyroid hormones can be measured directly and are usually decreased. • However, in early hypothyroidism, the level of thyroid hormones (T3 and T4) may be normal.
- 82. • Therefore, the main tool for the detection of hyperthyroidism is the measurement of the TSH, the thyroid stimulating hormone. • As mentioned earlier, TSH is secreted by the pituitary gland. • If a decrease of thyroid hormone occurs, the pituitary gland reacts by producing more TSH and the blood TSH level increases in an attempt to encourage thyroid hormone production. • This increase in TSH can actually precede the fall in thyroid hormones by months or years • Thus, the measurement of TSH should be elevated in cases of hypothyroidism.
- 83. • Third generation thyroid stimulating hormone (TSH) assays are readily available and are generally the most sensitive screening tool for primary hypothyroidism. • The generally accepted reference range for normal serum TSH is 0.40 – 4.2 mlU/L. • If the levels are above the reference range then the next step is to measure free Thyroxine (T4). • Patients with primary hypothyroidism usually have elevated TSH levels and decreased free hormone levels. • In patients with hypothalamic or pituitary dysfunction, TSH levels do not increase in appropriate relation to the low free T4 levels
- 84. treatment • With the exception of certain conditions, the treatment of hypothyroidism requires life-long therapy. • Before synthetic levothyroxine (T4) was available, desiccated thyroid tablets were used. • Desiccated thyroid was obtained from animal thyroid glands, which lacked consistency of potency from batch to batch. • Presently, a pure, synthetic T4 is widely available. Therefore, there is no reason to use desiccated thyroid extract.
- 85. • As described above, the most active thyroid hormone is actually T3. • So why do physicians choose to treat patients with the T4 form of thyroid? • T3 [liothyronine sodium (Cytomel)] is available and there are certain indications for its use. • However, for the majority of patients, a form of T4 [ levothyroxine sodium (Levoxyl, Synthroid)] is the preferred treatment. This is a more stable form of thyroid hormone and requires once a day dosing, whereas T3 is much shorter-acting and needs to be taken multiple times a day. • In the overwhelming majority of patients, synthetic T4 is readily and steadily converted to T3 naturally in the bloodstream, and this conversion is appropriately regulated by the body's tissues.
- 86. • The average dose of T4 replacement in adults is approximately 1.6 micrograms per kilogram per day. • This translates into approximately 100 to 150 micrograms per day. • Children require larger doses. • In young, healthy patients, the full amount of T4 replacement hormone may be started initially. • In patients with preexisting heart disease, this method of thyroid replacement may aggravate the underlying heart condition in about 20% of cases
- 87. • In older patients without known heart disease, starting with a full dose of thyroid replacement may result in uncovering heart disease, resulting in chest pain or a heart attack. • For this reason, patients with a history of heart disease or those suspected of being at high risk are started with 25 micrograms or less of replacement hormone, with a gradual increase in the dose at 6 week intervals. • Ideally, synthetic T4 replacement should be taken in the morning, 30 minutes before eating. • Other medications containing iron or antacids should be avoided, because they interfere with absorption
- 88. • Therapy for hypothyroidism is monitored at approximately six week intervals until stable. • During these visits, a blood sample is checked for TSH to determine if the appropriate amount of thyroid replacement is being given. • The goal is to maintain the TSH within normal limits. Depending on the lab used, the absolute values may vary, but in general, a normal TSH range is between 0.5 to 5.0uIU/ml. • Once stable, the TSH can be checked yearly. • Over-treating hypothyroidism with excessive thyroid medication is potentially harmful and can cause problems with heart palpitations and blood pressure control and can also contribute to osteoporosis. • Every effort should be made to keep the TSH within the normal range.
- 90. Levothyroxine (LT4) • Generally considered to be the treatment of choice for patients with hypothyroidism. • DOSING: • MILD HYPOTHYROIDSM • 1.7 mcg/kg or 100 – 125mcg/day • Not to exceed 300 mcg/day • SEVERE HYPOTHYROIDSM • INITIAL: 12.5 – 25 mcg PO qDay • Adjust dose by 25 mcg/day q 2 – 4wks PRN • MYXEDEMA COMA • 200 – 500mcg IV once • Then 100 – 300mcg 1 day later PRN
- 91. Thank you!!
