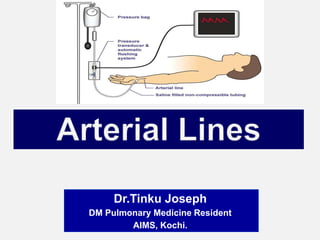
Arterial lines by Dr.Tinku Joseph
- 1. Dr.Tinku Joseph DM Pulmonary Medicine Resident AIMS, Kochi.
- 2. Indications Preparation & Equipments Positioning Insertion Complications Mechanism of Action Troubleshooting
- 3. An arterial line is an invasive method to measure BP.
- 5. 1.Continuous, beat-to-beat blood pressure measurement. - Hemodynamically unstable pts /ICU pts requiring inotropic support - Patients undergoing major surgery 2.Frequent arterial blood gas analysis -pts with respiratory failure on ventilator -severe acid/base disturbance.
- 6. 3. Facilitation of reliable titration of vasoactive medications. 4. Unable to obtain non invasive BP.
- 7. 1) Known deficiencies in collateral circulation: Raynauds phenomenon, Thromboangitis obliterans, Brachial artery insufficiency. 2) Infection of the site. 3) Trauma to the proposed site. 4) Excessive anticoagulation.
- 8. Advantages of IBP measurement Continuous blood pressure recording Accurate blood pressure recording even when patients are profoundly hypotensive vs NIBP which is difficult or inaccurate Real time Visual Display Disadvantages of IBP measurement Potential complications Skilled technique reqd Expensive
- 9. The radial artery has low complication rates compared with other sites. It is a superficial artery which aids insertion, and also makes it compressible for haemostasis The ulnar, brachial, axillary, dorsalis pedis, posterial tibial, femoral arteries are alternatives.
- 10. The idea here is to figure out if the ulnar artery will supply the hand with enough blood, if the radial artery is blocked with an a-line. Allen’s test is recommended before the insertion of a radial arterial line. This is used to determine collateral circulation between the ulnar and radial arteries to the hand If ulnar perfusion is poor and a cannula occludes the radial artery, blood flow to the hand may be reduced. The test is performed by asking the patient to clench their hand. The ulnar and radial arteries are occluded with digital pressure. The hand is unclenched and pressure over the ulnar artery is released. If there is good collateral perfusion, the palm should flush in less than 6 seconds.
- 11. Arterial cannula Made from polytetrafluoroethylene (‘Teflon’) to minimize the risk of clot formation 20G (pink) cannula - adult patients 22G (blue)- paediatrics 24G (yellow) - neonates and small babies Larger gauge cannulae increase the risk of thrombosis, smaller cannulae cause damping of the signal. The cannula is connected to an arterial giving set.
- 14. ARTERIAL SET - Specialized plastic tubing, short and stiff to reduce resonance, connected to a 500 ml bag of saline. SALINE BAG -500 ml 0.9% saline pressurized to 300 mmHg using a pressure bag, i.e. a pressure higher than arterial systolic pressure to prevent backflow from the cannula into the giving set. -The arterial set and pressurized saline bag with 2500units Heparin incorporate a continuous slow flushing system of 3–4 ml per hour to keep the line free from clots. -The arterial set and arterial line should be free from air bubbles. - The line is attached to a transducer.
- 15. DO NOT ALLOW THE SALINE BAG TO EMPTY –To maintain patency of arterial cannula. –To prevent air embolism –To maintain accuracy of blood pressure reading –To maintain accuracy of fluid balance chart –To prevent backflow of blood TRANSDUCER, AMPLIFIER AND ELECTRICAL RECORDING EQUIPMENT. -The transducer is zeroed and placed level with the heart.
- 16. Tape and/or steri-strips An arm board or towel roll Opsite or Tegaderm cover dressing Local anesthetic (1% or 2% lidocaine ,lidocaine cream) Suture material for femoral arterial line placement (2.0 silk) Scissors Monitor cable for transducing arterial waveform. Benzoin solution
- 18. 1. Ensure that all pre-procedure steps are taken 2. Pressure tubing with transducer is connected to bedside monitor. 3. Perform the Allen’s test to ensure adequate collateral blood flow. 4. Wash hands and wear gloves 5. For the radial artery, the arm is restrained, palm up, with an arm board to hold the wrist dorsiflexed
- 19. For the radial artery, the most common insertion site, the arm is restrained, palm up, with an armboard to hold the wrist dorsiflexed
- 20. 6. Apply anesthetic agent (local lidocaine 1-2% or lidocaine cream). 7. Locate pulsating artery via palpation. 8. Cleanse area selected for arterial line placement. 9. Prepare patient for puncture. 10. Stabilize artery by pulling skin taut. 11. Puncture skin at 45-60 degree angle for radial artery; 90 degrees for femoral artery.
- 21. 12. Advance catheter when flash of blood is observed in catheter. 13. Connect to pressure I.V. tubing and check for arterial waveform on bedside monitor. 14. Cleanse area of any blood and allow site to dry. 15. Apply Benzoin to cleansed area and allow to dry. 16. Secure arterial line with tape and cover with a Tegaderm dressing. 17. Secure I.V. tubing to prevent it from being caught and pulling on arterial catheter. If a femoral arterial line is placed, it should be secured with a suture. 18. Properly dispose of the I.V. sharps and other used materials.
- 22. 1. Direct cannulation 2. Transfixation 3. Guidewire (Seldinger) technique
- 25. Haemorrhage may occur if there are leaks in the system. Connections must be tightly secured. Emboli. Air or thrombo emboli may occur. Care should be taken to aspirate air bubbles Accidental drug injection may cause severe, irreversible damage to the hand. -No drugs should be injected via an arterial line - The line should be labelled (in red) to reduce the likelihood of this occurring
- 26. Arterial vasospasm Partial occlusion due to large cannula width, multiple attempts at insertion and long duration of use Permanent total occlusion Sepsis or bacteraemia secondary to infected radial arterial lines is very rare (0.13%); -local infection is more common. -if the area looks inflamed the line site should be changed.
- 31. Concentration of a drug into the tissues served by the cannulated artery can result in cell death Skin necrosis, severe gangrene, limb ischemia, amputation & permanent disabilities
- 32. Mechanism of action A transducer is a device that reads the fluctuations in pressure – it doesn’t matter if it’s arterial, or central venous, or PA The column of saline in the arterial set transmits the pressure changes to the diaphragm in the transducer
- 33. The transducer reads the changing pressure, and changes it into an electrical signal that goes up and down as the pressure does which is displayed as an arterial waveform. The transducer connects to the bedside monitor with a cable, and the wave shows up on the screen, going from left to right.
- 35. The transducer has to sit in a “transducer holder” – this is the white plastic plate that screws onto the rolling pole that holds the whole setup. The transducer has to be leveled correctly-to make sure that it’s at the fourth intercostal space, at the mid- axillary line (Phlebostatic axis)
- 36. Make sure there’s no air in the line before you hook it up to the patient – use the flusher to clear bubbles out of the tubing. Zero the line to atmospheric pressure properly Choose a screen scale that lets you see the waveform clearly.
- 39. To ensure accuracy of readings Flush the device & turn it off to patient but open to atmosphere This exerts pressure on transducer This pressure is called zero Zero once per shift or if values are questionable Ensure flush bag is pumped up
- 40. Once inserted, an arterial waveform trace should be displayed at all times This confirms that the invasive arterial BP monitoring is set up correctly, and minimizes problems.
- 41. The highest point - systolic pressure, -the lowest is the diastolic. Everybody see the little notch on the diastolic down slope? – there’s one in each beat. A little after the beginning of diastole – the start of the downward wave – the aortic valve flips closed, generating a little back- pressure bump: called the “dicrotic notch”..
- 44. Now we know how the arterial pressure monitoring system works, we need to be able to decide whether or not the trace (and BP in numerical format) is accurate. Failure to notice this may lead to unnecessary, or missed treatments for our patients. There are 2 main abnormal tracing problems that can occur once the monitor gain is set correctly.
- 45. Dampened trace
- 46. Dampening occurs due to: • air bubbles • overly compliant, distensible tubing • catheter kinks • clots • injection ports • low flush bag pressure or no fluid in the flush bag • Improper scaling • Severe hypotension if everything else is ruled out This type of trace Under estimate SBP, over estimate DBP
- 47. Resonant trace
- 48. Resonance occurs due to: • long tubing • overly stiff, non-compliant tubing • increased vascular resistance • reverberations in tubing causing harmonics that distort the trace (i.e. high systolic and low diastolic) • not-fully opened stopcock valve This type of trace: Over estimate SBP, under estimate DBP
- 49. Arterial lines measure systolic BP approximately 5 mmHg higher and the diastolic BP approximately 8 mmHg lower compared to non- invasive BP (NIBP) measurement.
- 59. “It takes a year just to learn which way to turn the stopcocks!” This is really true: some stopcocks point to where they’re open, and some point to where they’re closed – it just takes some time to learn which is which. The trick is remembering which way to turn the stopcock, and avoiding a mess. Don’t forget to clear the stopcock, recap, and then flush the line. Keep things nice and sterile.
- 60. This probably means that the artery being monitored gone into spasm. You need to think about things that might make this happen: -Is the patient very cold? -Are his extremities poorly perfused? -Is he on a “shipload” of pressors, making his arterial bed tighten up – - Is he “dry” as well? Sometimes arteries become unhappy with catheters in them, and you just have to convince the team that the patient needs a new one placed in another site.
- 61. The first thing to think about is: 1.Is the arterial catheter still in place? Yes? Try drawing with a 3cc syringe from the stopcock – if it draws normally, then you’ve got a hardware problem 2.Cables become loose? 3.Did the screen scale get accidentally set to, say, 40, instead of 150 or 200mm of pressure?- you’ll only see a flat line. 4.Is it a transducer setup Failure – try a new setup. If the line doesn’t draw – -Is there a clot in the hub? -Try taking the site dressing down – is the catheter kinked going into the patient? - Sometimes art-lines just fail – the artery spasms and won’t open up – time for a new site.
- 62. The routine now is 96 hours – make sure that you label the line setup when you hang it. Obviously, change the line setup if it is contaminated in any way.
- 63. Usually this will be pretty obvious: the pulse will diminish, or go away altogether. The hand may look dusky, or be cold, or lose some sensation – remember to assess for coloring, sensation, motion, and capillary refill. If you think that the a-line is threatening the patient’s hand, let the team know right away, and be ready to set up for another insertion somewhere else if the line is still necessary.
- 64. Compress the site with a sterile 4x4 for at least 5 minutes, or longer if the patient is anticoagulated. Assess the perfusion of the hand. Make sure you put the patient on the non- invasive cuff at meaningful intervals while you talk to the team about replacing the line
- 65. This is usually pretty obvious – the patient is hemodynamically stable, needs only one or two blood draws in a day, no more need for ABGs
- 66. Disconnect the cable from the monitor which will automatically turn off the alarms. Take out the sutures in the usual way with a fresh sterile kit. Have a gauzepiece ready, pull the catheter, and manually compress the site for at least 3 to 5 minutes. Make sure the patient’s hand is still perfused. Check for hematoma or bleeding, put a compression dressing on the site (not too tight!), which you can then take off after about an hour. Recheck the site hourly for a few hours afterwards – a hematoma could still form, and since there isn’t a whole lot of room in a wrist, you’d definitely want to know!
