Bonepresentationgeneral.compressed
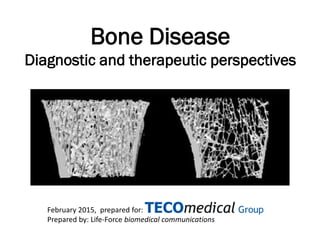
- 1. Bone Disease Diagnostic and therapeutic perspectives February 2015, prepared for: Prepared by: Life-Force biomedical communications
- 2. Contents Bone structure & function Bone proteins Bone metabolism & disease Bone disease therapies Bone disease biomarkers Bone biomarker response to therapy Pre-analytical requirements for Dx use of biomarkers
- 3. Bone function • Rigid framework to protect vital organs. • Muscle attachment, allows movement. • Hematological: home of bone marrow. • Central role in Calcium and Phosphate homeostasis –85-90 % of phosphate –99% of calcium is stored in the bones and teeth
- 4. Bone content • < 70% Bone Mineral: Ca10(PO4)6(OH)2, combine and harden the matrix into hydroxyapatite crystals • > 10% water • < 20% organic • 85% Type I collagen fibres • non-collagenous proteins like osteopontin, osteocalcin • proteoglycans • growth factors like IGFs, TGF-ß, PDFGs, BMPs (Ca10(PO4)6(OH)2)
- 5. Bone collagen type 1 major organic bone component • The basic structural unit is a triple helix molecule. • In fibres collagen molecules pack together side by side. • Crosslinks between the chains and between the molecules give collagen its strength. N N C Pyridinium crosslink helical region telopeptide region { { C
- 6. Bone collagen crosslinks • Found almost exclusively in bone collagen – PYD in cartilage, bone and ligaments; DPD in bone and dentin – Released into circulation as a result of collagen degradation during bone resorption
- 7. Bone architecture –Cortical bone Comprises ~80% of bone mineral mass Shafts of long bones and outer surfaces of flat bones Mechanical strength increases with thickness –Trabecular bone Comprises ~80% of bone surfaces Mainly at ends of long bones and inside flat bones and vertebrae Mechanical strength determined by number & thickness of trabeculae, and nr. of horizontal connections More rapidly affected by increased bone turnover
- 8. Bone - Calcium & Phophate metabolism Skeleton (storage), Gut (uptake), Kidney (secretion). • Parathyroid hormone (PTH): Action = Ca increase in blood • stimulates bone resorption (osteoclasts) • stimulates renal reabsorption of Ca • stimulates synthesis active vit D • 1,25-dihydroxyvitamin D: Action = Ca (& Pi) increase stimulates Ca and Pi uptake from food (through gut) • Calcitonin (CT): Action = Ca decrease • counteracts all PTH actions • inhibits bone resorption (osteoclasts) and renal reabsorption • Fibroblast Growth Factor, FGF23: Action = Pi decrease reduces renal reabsorption of Pi, inhibits synthesis active 1,25 vit D
- 9. Bone turnover • Bone resorption (osteoclasts digest type I collagen) and bone formation (osteoblasts) is ongoing dynamic process. • Normally balanced, 10% skeleton renewal per year.
- 10. Bone turnover – cellular players • Osteoblast Cell: • Formation, organization & mineralization of bone matrix. • Synthesis of collagen and other bone proteins. • Osteoclast Cell • Responsible for mineral dissolution (by acid environment and lysozymal enzyme action below ruffled border). • Responsible for collagen break down (Cathepsin K and MMP pathways).
- 11. Bone turnover – cellular players • Osteocyte or star-shaped cell • Most abundant cell in cortical bone • Result from osteoblasts trapped in the matrix they secrete • Networked to each other via long cytoplasmic extensions • Function as key mechanosensors • Destroys bone through a rapid mechanism called osteocytic osteolysis
- 12. Osteocytes star shaped cells sense mechanical loading this inhibits sclerostin expression which indirectly stimulates bone formation
- 14. Bone proteins - collagenous Bone formation Bone resorption Collagen synthesis metabolites Type I procollagen N-terminal propeptide (PINP) C-terminal propeptide (PICP or CICP) Type I collagen Collagen breakdown products DPD (Deoxypyridinoline) PYD (Pyridinoline) NTX (Cross-linked N-terminal telopeptide) CTX (Cross-linked C-terminal telopeptide) ICTP (Carboxy-terminal telopeptide) Helical peptide
- 15. Bone proteins non-collagenous bone formation role/function Protein Bone formation function Bone specific alkaline phosphatase (BAP) Osteoblastic enzyme involved in bone formation (probably plays a role in bone matrix maturation). Osteocalcin (OC) or Bone gla protein Major structural protein of the bone matrix, binds calcium and attracts osteoclasts. Matrix gla protein (MGP) Found in in bone, heart, kidney and lung. In bone, its production is increased by vitamin D. Like OC a calcium binding protein. Osteonectin Binds calcium and is involved in regulation of mineralization. Proteoglycans Role is unclear. Bone Sialo Protein (BSP) Major structural protein of the bone matrix. Its role has been associated with mineral crystal formation. Sclerostin Synthesized by osteocytes, inhibits bone formation by regulating osteoblast function and promoting osteoblast apoptosis.
- 16. Bone proteins non-collagenous bone resorption role/function Protein Bone resorption function Tartrate resistant isoenzyme acid phosphatase (TRAP5b) Synthesized by active osteoclasts. TRAP5b catalyzes the formation of reactive oxygen species (ROS), that degrade bone matrix products in resorbing osteoclasts. Cathepsin K Main osteoclastic protease, responsible for bulk degradation of Type I Collagen. Matrix Metallo Proteinases (MMPs) MMP-2, -9, -13, -14 participate in the degradation of the collagenous bone matrix, resulting in epitope ICTP. Lysozymal enzymes Enzymes secreted by the osteoclasts, responsible for mineral dissolution in an acid environment. Calcitonin receptor Osteoclastic receptor for calcitonin, an inhibitor of osteoclast activity. RANK(NF-κB ) Osteoclastic receptor for sRANKL Osteopontin Cell-binding protein, synthesized by otstoblasts, that anchors osteoclasts to mineralised matrix. sRANKL Soluble Receptor Activator of Nuclear Factor (NF)-κB Ligand. Binds to RANK and is the main stimulatory factor for the formation of mature osteoclasts. OPG (Osteoprotegerin) OCIF (Osteoclast Inhibiting Factor) OBF (Osteoclast Binding Factor) Key factor in inhibition of osteoclast differentiation and activity. Binds and acts as as decoy receptor for s-RANKL.
- 17. Bone formation stimulators & inhibitors Protein Stimulation Inhibition Systemic • PTH • PTHrP • Sex-steroids E2,T) • Growth hormone • IGF-1 • Thyroid hormone • Leptin • Glucocorticoids • β-2 adrenergic • Leptin • Serotonin Local • Transforming growth factor-ß • BMP-2 • Platelet-derived growth factors • Endothelial growth factor (EGF) • Vascular EGF • IGF-1 • Fibroblast growth factors (FGF-2) • Prostaglandins • Wnt-LRP5/6 • Sclerostin • Noggin • Interleukin-1ß,7 • Interferon- Ƴ • Tumor necrosis factors • Dickkopfs (DKK-1)
- 18. Bone resorption stimulators & inhibitors Protein Stimulation Inhibition Systemic • PTH • PTHrP • 1,25 (OH2)D3 • Thyroid hormone • β-2 adrenergic • Calcitonin • Sex steroids (Estrogen, Testosterone) Local • RANKL • Macrophage-CSF • Granulocyte macrophage-CSF • Interleukin-1,6,7,11,15,17 • Interferon-Ƴ • Tumor necrosis factor-α (TNF-α) • Fibroblast growth factors • Prostaglandins • Osteoprotegerin (OPG) • Transforming growth factor-ß (TGF-β) • Interferon-Ƴ • Interleukin-4,10, 13,18 • Interleukin-1 receptor antagonist
- 20. Bone disease • Aging, disease or other conditions may cause imbalanced bone resorption/formation, processes occur at different rates. • Osteoporosis is the main clinical bone disease (low bone mass & structure deterioration), affects 1/3rd of women 60- 70 years, and 2/3rd aged > 80. Men Women 20 40 60 80 Fracture Zone Years Bonemass
- 21. Osteoporosis pathogenesis * Reproduced from Graham Russell, with permission.
- 22. Metabolic bone disorders • Hyperparathyroidism • Hyperthyroidism • Renal failure • Vitamin D disorders • Paget’s disease • Metastatic cancer to bone • Nutritional rickets • Osteomalacia • Multiple myeloma • Malabsorption syndrome • Systemic lupus erythematosus (SLE). • Prolonged immobilization
- 23. Drug-induced bone disorders • Immunosuppressive drugs • Heparin, used in kidney dialysis • Phenytoin for epilepsy • Glucocorticoids (corticosteroids) for rheumatoid arthritis • Glucocorticoids (corticosteroids) for asthma • Aluminium intoxication • Vitamin A intoxication • Thiazide use.
- 24. Bone disease therapies - summary • Non-pharmalogical: – diet/supplements/exercise/prebiotics…. • Agents inhibiting resorption: – Bi(s)phosphanates – Hormone replacement therapy (HRT) • Agents stimulating bone formation: – PTH – Growth factors • Agents inhibiting resorption and stimulating formation – Strontiumranelate • Biologicals: – Monoclonal antibodies or small biomolecules affecting resorption or formation
- 25. Bone disease therapies *A combination of prebiotic short- and long-chain inulin-type fructans enhances calcium absorption and bone mineralization in young adolescents Steven A Abrams, Ian J Griffin, Keli M Hawthorne, Lily Liang, Sheila K Gunn, Gretchen Darlington and Kenneth J Ellis American Journal of Clinical Nutrition, Vol. 82, No. 2, 471-476, August 2005 Therapy Application Non-Pharmacological approaches Nutrition Sufficient protein, calcium and vitamin D intake is recommendable for all ages. A good diet shortens hospital stay after hip fracture. Inulin: daily consumption of a combination of prebiotic short- and long-chain inulin-type fructans significantly increases calcium absorption and enhances BMD during pubertal growth* Exercise Regular exercise reduces risk of ostoperosis and delays decrease BMD. High-charge exercise increases BMD at hip + forearm. Fall prevention Smoking Cessation Smoking is osteoporosis risk factor. Cessation may have positive effect on BMD. Calcium and Vitamin D Calcium Prevention osteoporosis Vitamin D (calitriol) Active form of vitamin D given to post-menopausal women who have osteoporosis in the spine.
- 26. Bone disease therapies Therapy Application Anti bone-resorption agents Inhibit bone resorption and increase mineral density. Actions reduce loss of bone mineral, leading to increased mineralization and mineral density. Decreased fracture rate during first 5 years. No rebuilding of bone that is lost in osteoporosis. Hormone replacement Estrogen Use for shortest time at start of menopause, prolonged use increase breast cancer and cardiovascular risks. Tibalone Increases BMD effectively. However, significant increase of risk of stroke. Selective estrogen receptor modulators Prevent bone loss and increase BMD (Raloxifene, (Evista)) Phytoestrogen Natural source of estrogen as found in soy. Used by women as a “safe”alternative to HRT. Biphosphanates (Alendronate (Fosamax); Risedronate (Actonel), Ibandronate, Zoledronic acid). Prevent bone loss and increase BMD. Rigid administration is disadvantage. Under FDA review, because of alleged risks for long-term use by post-menopausal women Calcitonin (Miacalcin) Treatment of osteoporosis and Paget's disease, considered not as effective as biphosphanates. Decreased tolerance with long-term use (nasal spray)
- 27. Bone disease therapiesTherapy Application Bone-formation stimulating agents Sodium floride Increases BMD, however, clinical studies showed no decrease in vertebral fracture ratesf Parathyroid hormone (PTH ) analogue (Teriparatide; Forteo) PTH increases bone turnover, and it increases formation of bone more than resorption. Results in new bone formation; a laying down of protein matrix and mineralization, occurring in the previous existing matrix, but also in the new structure. Treatment of osteoporosis. PTH increases spinal bone density and hip bone density. The relative risk of having moderate vertebral fracture is greatly reduced . Growth factors Growth hormone therapy is used (and FDA approved) in the treatment of hypopituitarism and somatotropin deficiency of children and adults. Agents inhibiting bone resorption and stimulating bone formation: Strontiumranelate (Protelos; Servier) Registered as a prescription drug in > 70 countries for treatment of post-menopausal osteoporosis to reduce risk of vertebral and hip fractures. In US, not approved by the FDA. Biologicals: Antibody to Sclerostin (Amgen, AMG-785) Stimulates bone formation, Increases markers of bone formation in post-menopausal women Sclerostin small molecule inhibitors (OsteoGeneX Inc.) As above human monoclonal anti s-RANKL antibody, inhibits bone resorption (Denosumab, AMGEN) Approved by FDA for use in postmenopausal women with risk of osteoporosis in June 2010
- 28. Diagnosis of bone disease • Measurement of Bone Mineral Density (BMD) at hip and/or spine is the gold standard. • BMD reflects bone history, it is not predictive. • Detectable changes in BMD take years to develop. • BMD does not provide information on deterioration of bone tissue architecture. • Increasing number of drugs therapies available for treatment requires use of rapid and predictive methods to diagnose disease and to assess the efficacy of therapy. • All biochemical players of bone metabolism are potential biomarkers.
- 29. Bone disease biomarkers • Elucidation of bone resorption and formation processes has offered many biomarker candidates. • Ideal bone disease biomarkers should demonstrate: • Differences pre-and post-menopause • Significant changes in response to treatment • Detect changes in short time intervals (months) • Minimal analytical variation • Minimal within person variation • Preferably little variation over the day • Preferably high stability in specimen
- 30. Main routine biomarkers of Bone Turnover & Calcium/Pi metabolism BONE FORMATION • BAP • Osteocalcin BONE RESORPTION • CTX-I • NTX-I CALCIUM METABOLISM • PTH • 25 vitamin D • 1,25 vitamin D • Calcium • Calcitonin SPECIAL SITUATIONS • TRAP5b (dialysis patients) • Sclerostin (osteocyte function) • OPG/sRankl (regulation of bone turnover) Pi METABOLISM • FGF23
- 31. Therapy monitoring using biomarkers hormone replacement therapy (HRT) - BAP • Mean BAP decreased 32% from baseline after 12 months in HRT- treated women, a significant difference from placebo group HRT Placebo Months of Therapy BAP (U/L) 10 15 20 25 0 12 24 36 International Osteoporosis Foundation (IOF) recommendation: for a 90 % specificity to predict a positive BMD response (+3 %), BAP value of an individual patient should decrease 20 to 40 % from the baseline value. Data on file, Metra Biosystems; source: Merck Research Laboratories.
- 32. Therapy monitoring using biomarkers hormone replacement (HRT) and biphosphanate therapy– Osteocalcin (OC) Greenspan, S. L. et al. J Clin Endocrinol Metab 2005;90:2762-2767
- 33. Therapy monitoring using biomarkers hormone replacement therapy (HRT) - DPD Months of Therapy Dpd Spine BMD BMD % ∆ Dpd % ∆ -1 0 1 2 3 0 3 6 9 12 -30 -20 -10 0 Hip BMD Postmenopausal women treated with hormone replacement therapy Rosen et al. J Clin Endocrinol Metab 1997;82:1904; Chesnut et al. Am J Med 1997;102:29
- 34. Alendronate 10 mg/day Placebo Months of Therapy BAP (U/L) 6 8 10 12 14 16 0 3 6 9 12 Therapy monitoring using biomarkers biphosphanate therapy - BAP • Mean BAP decreased 31% from baseline after 3 months in BP treated women, reached nadir at 6 months, a 43% decrease. International Osteoporosis Foundation (IOF) recommendation: for a 90 % specificity to predict a positive BMD response(+3 %), BAP value of an individual patient should decrease 20 to 40 % from the baseline value. • Bettica P, Bevilacqua M, Vago T, et al. Short-term variations in bone remodeling biochemical markers: cyclical etidronate and alendronate effects compared. J Clin Endocrinol Metab 1997;82:3034-9
- 35. Therapy monitoring using biomarkers bisphosphonate therapy – BAP, OC, NTx, PYD Changefrombaseline(%) -100 -75 -50 -25 0 25 50 0 3 0 3 0 1 0 1 74% 35% 57% 57% BAP OC NTx Pyd * response (% change) exceeds long-term intra-individual CV of placebo-treated subjects (92% confidence level). Rosen et al. Calcif Tissue Int 1998:63:363-8 Months on Therapy
- 36. Therapy monitoring using biomarkers PTH therapy - BAP • PTH initially stimulates bone formation and later increases bone remodeling. Daily PTH treatment induced an increment in spinal BMD of 6.1 %. An increase of > 30 %. BAP at 3 months had a predictive value of more than 73 % for an increase in spinal BMD of at least 3 %. Over 15 months of therapy, BAP values had more than doubled (+116 % see Figure). Cosman F, Nieves J, Zion M, Woelfert L, Luckey M, Lindsay R. Daily and cyclic parathyroid hormone in women receiving alendronate. NEJM 2005; 353(6):566-75.
- 37. Therapy monitoring using biomarkers PTH therapy– CTX & OC Mean serum β-CTX increased with 180% from baseline to the 3rd month and 36% from baseline to 1st month, and 125% from the 1st to the 3rd month. Mean osteocalcin increased with 165% , from baseline to the 1st month with an additional increase (11%) from the 1st to the 3rd month. Isabel Oliveira de Sousa, Erik Trovão Diniz, Thyciara Fontenele Marques, Luiz Griz, Mário de Almeida Pereira Coutinho, Francisco Bandeira Arq Bras Endocrinol Metab. 2010;54/2 http://www.scielo.br/pdf/abem/v54n 2/23.pdf
- 38. Therapy monitoring using biomarkers PTH therapy - Sclerostin …………………. 0.00 0.20 0.40 0.60 0.80 1.00 0 5 10 15 SOST (ng/ml) hours after PTH injection Data on file, Tecomedical
- 39. Therapy monitoring using biomarkers TRAP5b during hemodialysis TRAP5b assay levels are unaffected by dialysis. In contrast serum NTX and osteocalcin decreased significantly after hemodialysis sessions (indication for accumulation in uremic serum), BAP increased slightly. Shidara K. et al. Serum levels of TRAP5b, a new bone resorption marker unaffected by renal dysfunction, as a useful marker of cortical bone loss in hemodialysis patients. Calcif Tissue Int. 2008 Apr;82(4):278-87. Epub 2008 Apr 18.
- 40. Therapy monitoring using biomarkers TRAP5b predialysis patients with chronic kidney disease TRAP5b in both CKD patient groups was significantly higher than the normal value of healthy individuals . Authors conclude that TRAP5b demonstrated superiority over NTX as a bone resorption marker.Assessment of bone metabolism in such patients using osteocalcin and NTX may in fact result in overestimation of bone turnover. Yamada S et al. Utility of serum tartrate-resistant acid phosphatase (TRACP5b) as a bone resorption marker in patients with chronic kidney disease: independence from renal dysfunction. Clin Endocrinol (Oxf). 2008 Aug;69(2):189- 96. Epub 2008 Jan 23.
- 41. Biomarker behavior in bone diseases
- 42. Biomarker response to various therapies Therapy Biomarker BAP Osteocalcin NTX-I CTX-I DPD TRAP5B Sclerostin Hormone replacement ▼ ▼ ▼ ▼ ▼ ▼ ▼ Biphosphonates ▼ ▼ ▼ ▼ ▼ ► PTH analogues ▲ ▲ ▲ ▲ ▲ ▼ Growth hormone ▲ ▲ Strontium ranelate ▲ ▲ ► ► Antibody to Sclerostin (Amgen, AMG-785) ▲ ▲ ▲► Sclerostin small molecule inhibitor (OsteoGeneX Inc.) Human monoclonal anti s-RANKL antibody, (Denosumab, AMGEN) ▼ Biomarker response is indicated as an increase or decrease from the baseline biomarker values (▲, increase; ▼, decrease; ►, no response or conflicting results reported by different studies; ▲►, initial increase, then return to baseline) so the biomarker value measured in the patient before onset of the therapy
- 43. Preanalytics Critical parameters in sample collection preceding Dx procedures.
- 44. Preanalytics for bone markers • Diurnal/daily variation determines time of sample collection • Effect of food intake or diet determines fasting before sample collection • Age dependent normal values • Sample type • Sample stability
- 46. Variation by age
- 47. Preanalytics for biomarkers Bone Marker Sample Type Sample preparation Sample stability Bone Formation BAP Serum, cell culture, heparine plasma Don’t treat with EDTA or citrate because of the inhibition of the BAP enzyme 2-8 ºC for storage ≤ 5 days -20 ºC for longer storage Osteocalcin Intact Serum, Heparin- or EDTA-Plasma Samples must be separated within 1 hour after blood collection 2-8 ºC for storage ≤ 4 hours -20°C for storage ≤ 3 years Osteocalcin (1-49) and (1-43), N-terminal & mid-regional Serum, Plasma Whole blood should be collected and must be allowed to clot for minimum 30 minutes at room temperature before the serum is separated by centrifugation (850 – 1500xg for 10 minutes). The serum should be separated from the clot within three hours of blood collection and transferred to a clean test tube. It is necessary taking care of the sample collection procedure to avoid haemolysis. Serum 2-8 ºC for storage ≤ 6 days ≤ -20 ºC for longer storage Stable ≤ 3 freeze/thaw cycles PINP (IDS) Serum, Plasma Samples should be separated as soon as possible after collection. 5 days (2-8°C) Avoid repeated freeze/thaw PICP/CICP Serum, Heparin- and EDTA Plasma, cell culture Avoid hemolysis of specimens 2-8 ºC for storage ≤ 5 days -20 ºC for longer storage Stable ≤ 3 freeze/thaw cycles DKK-1 Serum, cell culture Avoid lipemic or hemolyzed samples Before use, thaw samples at low temperature and mix thoroughly. Samples must be diluted 1:4 prior to use in the assay. An additional buffer and assay protocol is available for cell culture samples. Samples store at -20°C. Avoid repeated freeze/thaw cycles. BMP7 Serum
- 48. Preanalytics for biomarkers Bone Marker Sample Type Sample preparation Sample stability Bone Resorption NTX-serum Serum, cell culture - Collect sample in the morning or always at the same time of the day for each individual. 2-8 ºC for storage ≤ 24 hours -20 ºC for longer storage Stable ≤ 3 freeze/thaw cycles NTX-Urine Urine, cell culture Collect second morning urine or 24 hrs urine without adding preservatives Room temperature ≤ 24 hours 2°-8°C for storage ≤ 72 hrs Stable ≤ 3 freeze/thaw cycles CTX-Serum (Cartilaps) Serum, plasma Separate the serum from the cells within 3 hours after collection of blood. For optimal results it is recommended to draw blood as fasting morning samples. Freeze (<-20°C) samples immediately. CTX-Urine (Cartilaps) Urine Second morning void urine specimens, but any spot urine sample may be used. 4ºC for storage ≤ 24 hours -20 ºC for longer storage DPD Urine Cell culture Use preservative-free first or second morning urine. Collect specimens before 10 a.m. 2-8 ºC for storage ≤ 7 days -20°C for longer storage. Protect specimens from exposure to light. PYD Urine Cell culture Use preservative-free first or second morning urine. In case of longitudinal studies, urine should be collected at the same time every day 2-8 ºC for storage ≤ 7 days -20°C for longer storage. Protect specimens from exposure to light. Stable ≤ 3 freeze/thaw cycles
- 49. Preanalytics for biomarkers Bone Marker Sample Type Sample preparation Sample stability Bone Resorption PYD-serum serum Filter samples by adding 200 µl to a 30kMWCO Spin filter. Centrifuge 30 minutes at 3,000-10,000 x g. Protect filtrate from exposure to light. 2-8 ºC for storage ≤ 4 days -20°C for longer storage. Stable ≤ 3 freeze/thaw cycles Helical peptide Urine Cell culture Collect preservative-free urine. Collect before 10 a.m 2-8 ºC for storage ≤ 7 days ≤-20°C for longer storage Stable ≤ 4 freeze/thaw cycles ICTP (Orion) Serum recommended, plasma also possible. Do not use heparin or citrate plasma samples. 2-8 ºC for storage ≤ 5 days ≤-20°C for longer storage Avoid repeated freeze/thaw cycles. Cathepsin K Serum, cell culture Blood samples should be centrifuged within 90 minutes. Prior to assay, specimens should be well shaken 4 ºC for storage ≤ 2 days ≤-20° C (preferably -70° C) for longer storage Stable ≤ 4 freeze/thaw cycles Sclerostin Serum, cell culture Non-lipemic human serum Centrifuge collected blood samples within 4 hours Room temperature ≤ 3 days (serum) 2-8 ºC for storage ≤ 5 days ≤-20°C for storage ≤ 2 years ≤-80°C for longer storage Stable ≤ 3 freeze/thaw cycles TRAP (5b) Serum or plasma (Heparin) Room temperature ≤ 8 hours 2-8 ºC for storage ≤ 2 days ≤-20°C for storage ≤ 8 months ≤-80°C for longer storage Stable ≤ 3 freeze/thaw cycles
- 50. Preanalytics for biomarkers Bone Marker Sample Type Sample preparation Sample stability Bone Regulation OPG Plasma, serum Room temperature ≤ 8 hours 4 ºC for storage ≤ 2 weeks ≤-20°C for longer storage Serum is stable ≤ 3 freeze/thaw cycles Heparin plasma samples are not stable for multiple freeze/thaw cycles and should be aliquotted in individual vials to avoid freeze/thaw damage. sRANKL Serum, plasma (EDTA, Heparin), cell culture Thaw samples at low temperature and mix them thoroughly. Lipemic or hemolyzed samples may give erroneous results. Store samples at -20°C. For long-term storage store at -70 °C. Avoid repeated freeze/thaw cycles. Myostatin EDTA plasma, serum. Whole blood is not suitable. Untreated lipemic samples may produce incorrect results. Allow samples to come to room temperature (18 - 26 °C) and mix gentle, avoid foam formation.
- 51. Preanalytics for biomarkers Bone Marker Sample Type Sample preparation Sample stability Mineral metabolism (Ca++ & other) PTH-intact EDTA-Plasma, Serum EDTA plasma has been reported to demonstrate improved PTH stability as compared to serum Collect whole blood without anticoagulant or lavender [EDTA] tube. After allowing blood to clot, the serum or plasma should be promptly separated, preferably in a refrigerated centrifuge, ≤-20°C for storage if not tested same day Calcitonin Serum Collect whole blood without anticoagulant. After allowing blood to clot, the serum should be promptly separated, preferably in a refrigerated centrifuge. Avoid grossly hemolyzed or grossly lipemic samples. ≤-20°C for storage if not tested same day FGF-23 (intact) EDTA plasma or cell culture The intact FGF-23 molecule appears to be highly unstable resulting in decreased immuno-reactivity over time. Specimen collection and assay or storage procedures should be carried out in an expeditious manner. A morning, 12 hour fasting sample is recommended. Samples should be assayed immediately or stored frozen at -20ºC or below. Avoid repeated freezing and thawing of specimens. FGF-23 (C-terminal) Plasma, cell culture Centrifuge the sample and separate the plasma or media from the cells. Samples should be assayed immediately or stored frozen. ≤-20° C for storage Avoid repeated freeze-thaw cycles. 25-OH-Vitamin D Serum, cell culture 2-8 ºC for storage ≤ 24 hours ≤-20° C for longer storage Avoid repeated freeze/thaw cycles. 1,25-(OH)2- Vitamin D (Immundiagnostik) Serum, plasma Fresh collected blood should be centrifuged within one hour. Samples should be mixed well before assaying. Lipemic or hemolytic samples may give erroneous results. 2-8 ºC for storage ≤ 24 hours ≤-20° C for longer storage Avoid repeated freeze-thaw cycles. Serum samples can be shipped at 4-8 °C (for example with Coolpacks) and remain stable for up to 3 days Human soluble α-Klotho protein Serum, EDTA-plasma. Test samples should be measured soon after collection. Alternatively, freeze samples and upon use, thaw the samples at a low temperature and mix them completely before measurement. Store frozen and do not repeat freeze/thaw cycles.
